Bone Scans and Accuracy: How to Optimize Your Results
- osteostrongmissoul
- Oct 2, 2025
- 4 min read
By Rachel Ames, MPT, Owner and Operator OsteoStrong Missoula and Callie Trolson, Center Manager OsteoStrong Missoula
When it comes to monitoring bone health, even the smallest variations in testing can make a big difference in your results and what you do with them. That’s why consistency is key if you’re using DXA scans, and also why we’ve introduced Echolight REMS (Radiofrequency Echographic Multi Spectrometry) as a more reliable alternative and recommend it as your baseline.
Position Dependency
DXA scans require patients to lie in a very specific position. Even small changes in posture or alignment can alter the results, since DXA depends on capturing the bone from one fixed angle. Accuracy rests heavily on how the patient is positioned and how carefully the technician defines the scan boundaries.
REMS works differently. Using ultrasound waves with a handheld probe, it collects data dynamically from multiple angles around the bone. Because it doesn’t rely on one fixed position, fine adjustments are not needed. This minimizes human error, reduces variability between technicians, and produces clearer, more consistent measurements. In other words: the results you see reflect your true bone health, not positioning or operator variability.
Operator Dependency
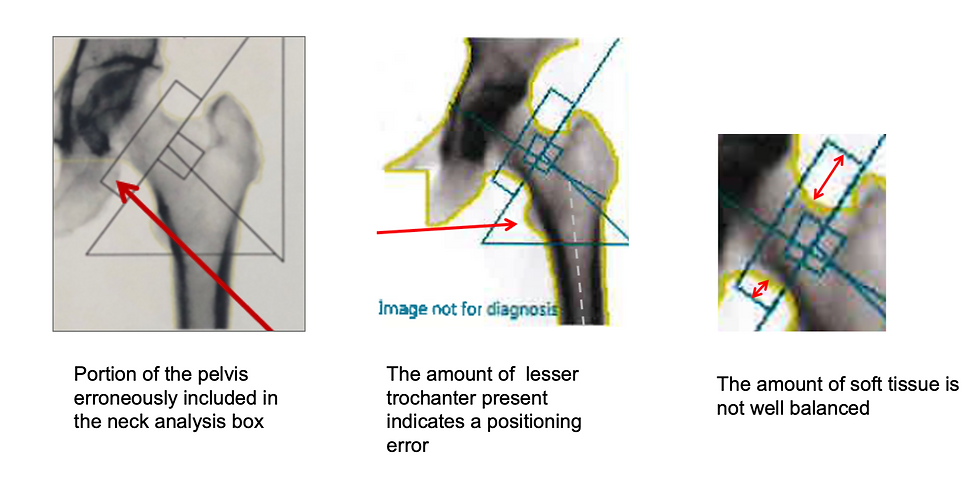
With DXA, the scanner software usually suggests boundaries for key areas of bone, called regions of interest (ROIs) — for example, specific vertebrae or parts of the hip. A well-trained technician must review these suggestions and often adjust them manually. If the boundaries are misplaced, other artifacts (ex: arthritis, calcifications, bone spurs) or the wrong vertebrae are selected, the results can be misleading. This is a common source of operator-related error with DXA. PubMed
DXA Scan

REMS uses ultrasound waves to “look” at your bones in real time. The software automatically identifies the ROIs and analyzes them — there’s no need for the technician to manually outline the bone like with an X-ray. The technician’s main job is simple: position the probe and capture a clear view of the bone on the screen. Once the image is captured, the REMS software does the rest automatically. This makes the scan faster, easier, and much less prone to human error, giving you more reliable results every time. PubMed2
REMS Scan

Precision and Least Significant Change:
You may have noticed a note on your bone scan reports indicating whether there has been a statistically significant change in your bone density over time. With DXA scans, there is a precision error of about 5%. This means that a gain or loss smaller than 5% may not reflect a true change in bone health—it could simply be a measurement error. REMS, on the other hand, has a much smaller precision error—around 1%. From this, technologists calculate the Least Significant Change (LSC), which is the threshold for deciding whether a difference in bone density is real or just error. This higher level of precision allows you to detect meaningful changes earlier, helping you make more informed decisions about your bone health.
Machine Dependency:
While the LSC helps confirm whether a change is real, it is tied to the specific machine and technician that performed the scan. With DXA, different machines—even from the same manufacturer—may give slightly different results due to calibration and software differences. Even if a facility replaces its DXA with a brand-new model from the same brand, the calibration will be different, and results may not line up exactly with prior scans. If you switch machines or operators, it can appear that your bone density changed when it really didn’t. That’s why DXA follow-ups are ideally performed on the same unit with the same technician, to make sure changes reflect your actual bone health, not differences in equipment. REMS reduces this problem by minimizing operator input and using automated analysis, which improves consistency across settings.

In Summary
While DXA has been the gold standard for many years, REMS provides distinct advantages: it’s position-independent, less error-prone, and more consistent across operators, machines, and time. REMS also provides a comprehensive quality measurement, reflecting bone strength and structure — not just density — which recent research is now confirming to be equally, if not more, important for fracture risk prediction. That’s why we recommend REMS as your lifelong baseline scan.
That said, when having a DXA scan, you can still improve accuracy by always using the same machine and technician. Doing so helps maintain the correct LSC reference and reduces variability, giving you a clearer picture of your bone health over time. If you have multiple DXA reports from different machines or technicians, they may be less directly comparable—but they can still serve as helpful data points. And remember—while scans are a valuable way to measure progress, they’re only one part of the bigger picture. At OsteoStrong, we focus on more than bone density, strengthening bone quality, balance, posture, and agility—so you can move with confidence, stay safe, and lower your risk of falls.
To dive deeper into these technologies, check out the video of our Strong Talk "Unlock Your Best Bone Health" here: https://vimeo.com/1010773025/11cdb03f96?fl=pl&fe=vl





